Alcoholic Liver Disease Explained Simply: Causes, Symptoms, Prevention, and Treatment

Medicine Made Simple Summary
Alcoholic liver disease is a condition caused by long-term excessive alcohol use that damages the liver. It begins with fat buildup in the liver and can progress to inflammation, scarring, and eventually liver failure if drinking continues, reflecting key aspects of alcoholic liver disease causes and treatment. The liver is responsible for processing alcohol, and repeated exposure overwhelms it, leading to injury. The most important treatment is complete abstinence from alcohol. When detected early and alcohol is stopped, the liver can heal significantly. Awareness, early diagnosis, and lifestyle changes are key to preventing serious complications.
What Is Alcoholic Liver Disease
Alcoholic liver disease, often shortened to ALD, refers to liver damage caused by long-term alcohol consumption. The liver breaks down alcohol, but excessive drinking over time overwhelms this process. As a result, harmful byproducts damage liver cells.
ALD does not happen overnight. It develops gradually, often silently, over years of drinking. Many people do not realize their liver is affected until damage becomes advanced.
Despite being preventable, alcoholic liver disease remains a major cause of liver failure worldwide.
Why Alcohol Damages the Liver
When alcohol enters the body, most of it is processed by the liver. During this process, alcohol is converted into toxic substances that injure liver cells. Repeated exposure causes inflammation and interferes with normal fat metabolism.
Alcohol also weakens the liver’s ability to repair itself. Over time, this leads to fat accumulation, cell death, and scarring. The more alcohol consumed and the longer it continues, the higher the risk of liver damage.
Stages of Alcoholic Liver Disease
Alcoholic liver disease develops in stages. These stages represent a continuous process rather than separate conditions.
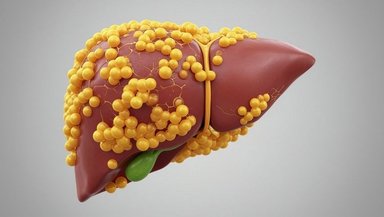
Fatty Liver Due to Alcohol
This is the earliest stage. Fat builds up inside liver cells due to alcohol metabolism, closely resembling fatty liver disease symptoms and prevention discussed in non-alcohol-related liver conditions. Most people have no symptoms at this stage.
Fatty liver caused by alcohol is reversible if drinking stops. Many people improve completely at this stage.
Alcoholic Hepatitis
Continued drinking leads to liver inflammation. This stage is more serious and can cause symptoms such as yellowing of the eyes, loss of appetite, fever, and abdominal pain.
Alcoholic hepatitis can range from mild to life-threatening. Even at this stage, stopping alcohol can improve outcomes.
Alcoholic Cirrhosis
This is the most advanced stage. Long-term injury leads to permanent scarring of the liver. Cirrhosis disrupts blood flow through the liver and reduces its ability to function.
Damage at this stage is largely irreversible and can lead to liver failure.
Who Is at Risk of Alcoholic Liver Disease
The main risk factor for ALD is long-term excessive alcohol consumption. However, not everyone who drinks heavily develops liver disease.
Factors that increase risk include high daily alcohol intake, female gender, poor nutrition, obesity, and viral hepatitis infections such as hepatitis C. Genetic differences also affect how individuals process alcohol.
Women are more vulnerable to alcohol-related liver damage even at lower levels of drinking.
Common Symptoms of Alcoholic Liver Disease
Early stages often cause no symptoms. As disease progresses, symptoms may become noticeable.
Common symptoms include fatigue, weakness, loss of appetite, nausea, and discomfort on the right side of the abdomen. These symptoms are often ignored or attributed to other causes.
In advanced disease, symptoms become more severe and may include yellowing of the skin or eyes, swelling of the abdomen or legs, easy bruising, confusion, and bleeding tendencies.
Why Symptoms Appear Late
The liver has a strong ability to function even when damaged. This means symptoms may appear only after significant injury has already occurred.
This delayed warning makes early screening and awareness especially important for people who drink regularly.
How Alcoholic Liver Disease Is Diagnosed
Diagnosis begins with a detailed history of alcohol use. Blood tests often show abnormal liver enzymes and changes in clotting and protein levels.
Imaging tests such as ultrasound can show fat accumulation or scarring. Special scans may assess liver stiffness.
In unclear cases, a liver biopsy may be done to confirm inflammation or scarring, though this is not always necessary.
Why Alcohol Abstinence Is Essential
Stopping alcohol completely is the most important step in treatment. No medicine can protect the liver if drinking continues.
Abstinence allows liver cells to recover and prevents further damage. In early stages, the liver can heal almost completely.
Even in advanced disease, stopping alcohol improves survival and quality of life.
Support for Stopping Alcohol
Quitting alcohol is difficult for many people and often requires support. Counseling, behavioral therapy, and support groups help maintain abstinence.
Some medications reduce cravings or help prevent relapse. Long-term success depends on sustained support and follow-up.
Alcohol dependence is a medical condition, not a personal failure.
Role of Nutrition in Recovery
Many patients with ALD suffer from poor nutrition. Alcohol interferes with nutrient absorption and appetite.
Adequate protein and calorie intake support liver repair. Vitamin deficiencies are common and often require supplementation.
Good nutrition improves immunity, energy levels, and overall recovery.
Medical Treatment for Severe Disease
In severe alcoholic hepatitis, doctors may use medications to reduce inflammation. These treatments are used carefully and only in selected cases.
Treatment decisions depend on disease severity and overall health. Close monitoring is essential.
Medicines support recovery but do not replace alcohol abstinence.
Managing Complications of Advanced Disease
Cirrhosis leads to complications that require ongoing medical care. These may include fluid buildup in the abdomen, bleeding from swollen veins, mental confusion, and infections.
Management focuses on symptom control and preventing further liver injury. Multidisciplinary care is often required.
Liver Transplantation
In end-stage liver disease, liver transplantation may be the only life-saving option. Candidates must demonstrate sustained abstinence from alcohol, usually for at least six months.
Transplantation offers excellent outcomes for selected patients but requires lifelong follow-up.
Prevention of Alcoholic Liver Disease
The most effective prevention is avoiding excessive alcohol use. Awareness about alcohol-related harm plays a key role.
Early screening for harmful drinking allows intervention before liver damage occurs. Vaccination against hepatitis viruses reduces additional liver stress.
Public policies that limit alcohol availability and promote responsible use help reduce disease burden.
Importance of Awareness and Early Action
Many people underestimate the harm caused by regular drinking. Education helps correct myths about “safe” alcohol levels.
Recognizing early symptoms and seeking medical advice can prevent progression to severe disease.
Alcoholic liver disease affects families and communities, not just individuals.
Living With Alcoholic Liver Disease
With abstinence and medical care, many people with ALD live meaningful lives. Improvement may be slow but steady.
Support from family, healthcare providers, and community programs makes recovery more achievable.
Hope and recovery are possible, especially when action is taken early.
Conclusion
Alcoholic liver disease is a serious but preventable condition caused by long-term excessive alcohol use. It often progresses silently until advanced stages, making awareness and early detection critical. Complete abstinence from alcohol is the cornerstone of treatment and can reverse early damage and improve survival even in advanced disease. With education, timely medical care, nutritional support, and strong social support, many people can halt disease progression and protect their liver health. Addressing alcoholic liver disease requires compassion, awareness, and collective responsibility.