Risks, Complications and What to Watch Out For After a Child’s Liver Transplant

Medicine Made Simple Summary
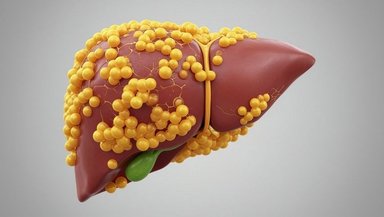
After a child’s liver transplant, the body needs time to adjust to the new liver. During this period, certain risks and complications may appear. The most common include rejection, infections, bile duct problems, blood clots, and issues caused by immunosuppressant medicines. Many of these complications are treatable when recognized early. Parents should watch for fever, jaundice, dark urine, tiredness, vomiting, abdominal swelling, and missed medication doses. Understanding these risks helps families respond quickly and support safer healing during the first year of recovery as part of the overall life after pediatric liver transplant journey.
Why Understanding Risks Helps Families Feel More Prepared
A pediatric liver transplant changes a child’s life. It replaces a damaged liver with a healthy one and restores many essential functions the body depends on. But the journey does not end once the surgery is complete. Recovery continues for months and even years. During this time, parents play a key role in monitoring symptoms, keeping up with medicines, and noticing early changes in their child’s health.
Learning about possible complications can feel worrying at first. But knowledge brings confidence. When parents understand what to expect throughout the pediatric liver transplant process, they can respond earlier, communicate better with doctors, and support stronger long-term outcomes. This article explains the main risks after transplant in simple, clear language so families feel equipped to guide their child through recovery.
The First Phase After Transplant: A Delicate Time for the New Liver
Why the Early Weeks Are So Important
The first few weeks after surgery are when the body adjusts to the new liver. The liver begins working immediately, but the immune system has not yet adapted. Medicines are being introduced. Surgical healing is happening. The child may be weak, swollen, or uncomfortable. For these reasons, doctors keep children under close observation.
Blood tests are done frequently to check liver function, blood flow, clotting ability, kidney health, infections, and medication levels. These tests help the medical team identify subtle changes before symptoms appear.
Common Signs Children Experience Early On
Children may continue to look jaundiced for a short time. Appetite may take a while to return. Some children are more tired than usual. These changes can be normal but must be monitored carefully. If symptoms worsen, the team steps in to find the cause quickly.
Rejection: The Body’s Defense System Responding to the New Liver
What Rejection Means in Simple Terms
Rejection does not mean the transplant is failing. It means the immune system recognizes the new liver as different and reacts to it. This is expected. Most children experience at least one rejection episode in the first year. These episodes are usually mild and respond well to medication adjustments.
Types of Rejection
Acute rejection
Happens in the first months after transplant. Usually reversible.
Chronic rejection
A long-term form of rejection that develops slowly. It is less common but more difficult to treat.
Symptoms Parents Should Watch For
Fever
New or worsening jaundice
Dark urine
Light-colored stools
Tiredness
Abdominal swelling
Reduced appetite
Parents who notice these symptoms should call the transplant team immediately. Rejection is easier to treat when found early.
Why Medication Timing Matters So Much
Immunosuppressants protect the liver from rejection. These medicines must be taken daily, at the same time, without missing doses. Even one missed dose can affect blood levels and increase the risk of rejection. Doctors help families create a routine that fits their schedule so doses are never forgotten.
Infections: Why Children Need Extra Protection After Transplant
Understanding Why Infection Risk Is High
Because immunosuppressants weaken the immune system, children are more likely to catch infections. These can be mild or serious depending on the type of germ and how early treatment begins. Infections may appear in the lungs, urinary tract, bloodstream, surgical site, or digestive system.
Some infections occur early, while others may appear months after transplant as medication levels change.
Early Signs of Infection
Fever
Chills
Cough
Vomiting
Diarrhea
Skin rashes
Sore throat
General weakness
Parents should report fever quickly, even if it seems mild. A fever may be the first clue that the immune system is struggling.
Preventing Infections at Home
Good handwashing
Avoiding contact with sick individuals
Following recommended vaccines as guided by the transplant team
Keeping the child away from crowded indoor spaces for a period after transplant
Ensuring clean food handling and safe drinking water
These simple habits help reduce infection risk during a sensitive time.
Bile Duct Complications: A Common Issue After Transplant
Why the Bile Duct Needs Special Attention
The bile duct is a narrow tube that drains bile from the liver into the intestine. During transplant, surgeons must reconnect this duct. Because the connection is delicate, problems may develop as the child heals.
Types of Bile Duct Complications
Bile duct stricture
A narrowing that slows or blocks bile flow.
Bile leak
Bile escapes into the abdominal cavity.
Bile obstruction
The duct becomes blocked completely.
Symptoms Families Should Watch For
New jaundice
Dark yellow urine
Pale chalky stools
Fever
Upper belly pain
Swollen abdomen
If bile cannot flow, it builds up in the liver and causes damage. Early treatment is important. Doctors may use imaging, endoscopy, stents, or surgery to correct these problems.
Blood Flow Problems: When Vessels Feeding the Liver Become Narrow or Blocked
Why Blood Vessels Are at Risk After Transplant
The liver relies on steady blood flow from the hepatic artery and portal vein. During transplant, surgeons carefully reconnect these vessels. Even so, clots or narrowing can develop, especially in young children with small blood vessels.
Serious Vascular Complications
Hepatic artery thrombosis
A clot in the main artery feeding the liver. This is an emergency.
Portal vein stenosis
Narrowing of the main vein carrying blood into the liver.
Hepatic vein obstruction
Blood cannot drain properly from the liver.
Warning Signs
Sudden increase in liver enzymes
Severe abdominal pain
Bleeding
Fluid buildup in the belly
Sudden weakness or collapse
These complications require urgent imaging and treatment.
Medication Side Effects: What Parents Should Expect and How to Manage Them
Why Medicines After Transplant Affect the Whole Body
Immunosuppressants keep the liver safe from rejection, but they also influence metabolism, kidneys, blood pressure, and growth. Regular monitoring allows doctors to catch side effects early. Children respond differently to medications, which is why individualized care and ongoing follow-up are important considerations when choosing a pediatric liver transplant center.
Common Medication Side Effects
Increased appetite
Weight gain
High blood pressure
High blood sugar
Kidney strain
Mood changes
Tremors
Extra hair growth
Increased infection risk
Children respond differently to medications. Doctors adjust doses based on age, weight, blood tests, and side effects.
How Families Can Support Healthy Medication Use
Keeping a written schedule
Using alarms
Monitoring for symptoms
Reporting side effects quickly
Encouraging healthy food choices
These steps help maintain safe medication levels.
Kidney Problems After Transplant
Why the Kidneys Need Careful Watching
Some immunosuppressants can stress the kidneys. Dehydration, infections, or other illnesses can increase this strain. Doctors check kidney function regularly through blood tests.
Early Signs of Kidney Stress
Low urine output
Swelling in legs or face
High blood pressure
Fatigue
Early treatment can prevent long-term damage.
Heart and Blood Pressure Changes After Transplant
Why Blood Pressure Often Rises
Certain medications, fluid balance changes, and healing stress can raise blood pressure. Good control protects the heart and kidneys. Doctors may recommend lifestyle adjustments or prescribe blood pressure medicine.
Nutrition and Growth After Transplant
Why Many Children Grow Quickly After Surgery
A healthy liver improves appetite, digestion, and nutrient absorption. Many children experience catch-up growth. Others may need support from dietitians if appetite remains low or if medications affect weight.
Nutrition Challenges Families May See
Poor appetite
Food intolerance
Vitamin deficiencies
Low muscle strength
Balanced meals, hydration, and follow-up with nutrition specialists help support healthy growth.
Emotional and Behavioral Health: An Overlooked Complication
Why Feelings Change After Transplant
A long hospital stay, pain, medicines, and disrupted routines can affect mood. Children may feel anxious, tired, or stressed. Teenagers may struggle with medication routines or frustration about restrictions.
When to Seek Help
Avoiding activities
Withdrawal
Frequent crying
Irritability
Trouble sleeping
Difficulty coping with hospital visits
Early support from psychologists or child-life specialists improves emotional well-being.
Warning Signs That Require Immediate Medical Attention
Parents should contact the transplant team urgently if the child has:
Fever
New jaundice
Dark urine or pale stools
Vomiting or severe diarrhea
Bleeding
Sudden tiredness
Confusion
Abdominal swelling
Pain that worsens
Missed medication doses
These symptoms could indicate rejection, infection, vascular problems, or bile duct issues.
The Importance of Lifelong Follow-Up
Why Transplant Care Never Truly Ends
A transplant offers a second chance at life, but it requires ongoing care. Children need regular clinic visits, blood tests, and medication checks. As they grow, doses change and new needs arise.
Preparing Children for Adulthood
Older children and teens learn how to
Take their own medications
Recognize warning signs
Make healthy lifestyle choices
Communicate with doctors
This helps them transition smoothly into adult transplant care one day.
Conclusion
If your child has undergone a liver transplant, maintain regular follow-up visits, monitor symptoms closely, and keep medication routines consistent. Call your transplant team whenever something feels unusual. Early action is the strongest protection for your child’s new liver and long-term health.
References and Sources
Pediatric Liver Transplant Program – CHOP
Liver Care – Nationwide Children’s Hospital