What Happens Before, During and After a Pediatric Liver Transplant — Step-by-Step Walkthrough for Parents

Medicine Made Simple Summary
A pediatric liver transplant is a journey with three major phases: the time before surgery, the surgery itself, and the recovery afterward. Before transplant, doctors perform tests, evaluate the child, and prepare families for donor options and timing, helping them understand what is pediatric liver transplant and how the process works. During surgery, the diseased liver is removed and replaced with a healthy donor liver. After surgery, the child recovers in the ICU, learns to take new medicines, and begins long-term follow-up. Understanding each step helps families feel prepared, informed, and confident throughout this complex but life-saving process.
Why Families Need a Clear Guide to the Transplant Journey
When parents first learn that their child needs a liver transplant, the most common questions are: What happens next? How long will this take? What does surgery involve? What will recovery look like? Many families also begin thinking about questions to ask before pediatric liver transplant as they try to make sense of urgent decisions. The process can feel overwhelming, especially when your child is already unwell. A clear, step-by-step understanding helps families replace fear with preparation. From the initial evaluation to long-term care, this article explains everything in straightforward language.
Understanding the Full Journey: Three Major Stages
- Before transplant
- During transplant
- After transplant
Each stage has its own steps, challenges, and goals. Together, they form the complete liver transplant pathway, often required for childhood liver diseases requiring transplant that cannot be managed with medicines or surgery alone.
Before the Transplant: Evaluation, Preparation, and Planning
The Initial Evaluation
The evaluation is designed to answer one question: Is a liver transplant the best and safest option for the child? This evaluation is detailed, because the transplant team must understand the child’s overall health, the severity of liver disease, and whether transplant will improve the child’s long-term outlook.
Evaluation includes
- Blood tests
- Imaging studies like ultrasound or MRI/CT
- Liver function tests
- Nutritional assessment
- Heart and lung evaluation
- Genetic or metabolic testing depending on diagnosis
Doctors review every organ system to ensure the child can tolerate surgery.
Meeting the Transplant Team
Families meet many specialists during this period: hepatologists, transplant surgeons, nurses, dietitians, pharmacists, psychologists, and social workers. Each one plays a role in preparing the family for the journey ahead.
Understanding Why a Transplant Is Needed
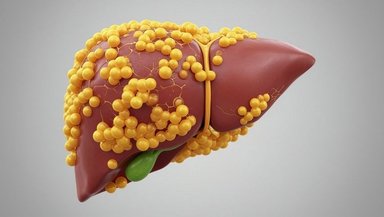
Doctors explain how the child’s liver disease affects the body and why other medical treatments are no longer enough. They describe how the transplant will help remove toxins, improve growth, support nutrition, and restore essential liver functions.
Choosing the Donor Type
Families learn about three donor options:
- Living donor
- Deceased donor
- Split liver transplant
Doctors explain which option fits the child best based on size, urgency, and medical condition.
Placement on the Waiting List
If the child needs a deceased donor liver, they are placed on a national waiting list. The waiting time varies based on urgency, size match, and donor availability. Some children may wait weeks; others may wait longer. Children with sudden liver failure are prioritized because they cannot wait safely.
If a living donor is available, surgery can often be scheduled sooner and when the child is medically stable.
Preparing Emotionally and Practically
This stage is stressful for families. Parents juggle medical appointments, monitor symptoms, and prepare for an uncertain timeline. Social workers and psychologists help families manage stress, plan logistics, and understand what to expect.
Warning Signs to Watch While Waiting
Increasing jaundice
- Swelling in the belly
- Bleeding easily
- Poor appetite
- Confusion or irritability
- Difficulty breathing
If these worsen, families should call their transplant team immediately.
During the Transplant: What Happens in the Operating Room
Arriving for Surgery
When the hospital calls to say a donor liver is available, families come to the hospital right away. For planned living donor transplants, families arrive at a scheduled time. The child undergoes a final physical exam and blood tests before surgery begins.
Understanding the Operating Room Process
The surgery usually takes six to ten hours. A large team participates, including transplant surgeons, anesthesiologists, nurses, perfusionists, and technicians.
Step 1: Anesthesia and Preparation
The child is given general anesthesia so they sleep throughout the procedure. The team places IV lines and monitors to track breathing, blood pressure, heart rate, and oxygen levels.
Step 2: Removing the Diseased Liver
Surgeons carefully disconnect the sick liver from the child’s blood vessels and bile duct. This is one of the most delicate steps because children’s blood vessels are very small.
Step 3: Implanting the Donor Liver
The new liver—whether from a living donor, deceased donor, or split graft—is placed inside the child’s abdomen. Surgeons connect the liver to major blood vessels so blood can flow into the new organ.
Step 4: Reconnecting the Bile Duct
The bile duct must be attached so bile can drain properly. Depending on the child’s anatomy, the surgeon may connect the bile duct directly to the intestine.
Step 5: Ensuring Blood Flow
The team checks that the liver receives steady blood flow. Once flow is established, the liver begins working immediately.
Step 6: Closing the Incision
The incision is closed in layers. In small children, the abdomen may be left partially open for a short time if swelling is expected. This is a normal part of pediatric transplant care in certain cases.
After Surgery
The child is moved to the pediatric ICU for close monitoring. Parents remain nearby and are updated throughout the surgery and recovery.
After the Transplant: Recovery, Healing, and Long-Term Care
The First Hours in the ICU
Right after surgery, doctors monitor
- Breathing
- Blood pressure
- Liver function tests
- Fluid balance
- Blood clotting
Most children wake slowly as anesthesia wears off. Some remain on the ventilator for a short time.
Pain Control and Comfort
Pain is managed with safe medications. Nurses monitor comfort closely, adjust settings, and keep the child calm and supported.
When the New Liver Starts Working
Many children show improved lab results within hours. Jaundice begins to fade. Urine output improves. The body starts responding to the presence of a healthy liver.
Removing Tubes and Lines
As the child stabilizes, drains, breathing tubes, and catheters are removed. Eating begins gradually. Nutritional support plays a big role in healing.
Starting Immunosuppression
To prevent the child’s immune system from attacking the new liver, daily medications called immunosuppressants are started. Families learn how to give these medicines and monitor for side effects.
Transition From ICU to Regular Hospital Room
Once stable, the child moves to a regular transplant unit where they begin physical therapy, start walking, and regain strength. Most children stay in the hospital for several weeks.
Understanding Rejection After Transplant
What Rejection Is
Rejection happens when the immune system recognizes the new liver as foreign and tries to attack it. This is a natural response, not a failure of the transplant.
Signs of Rejection
Rising liver enzymes
- Fever
- Jaundice
- Dark urine
- Fatigue
Most rejection episodes are mild and reversible with medication adjustments.
Life at Home After a Liver Transplant
Follow-Up Appointments
Children return to the transplant center frequently in the first few months. Blood tests help doctors adjust medications and watch for complications. Over time, visits become less frequent, and families gain confidence in managing daily life and routines associated with life after pediatric liver transplant.
Nutrition and Growth
Good nutrition helps the liver heal. Some children grow rapidly after transplant because their new liver finally supports healthy metabolism.
Infection Precautions
Because immunosuppressants weaken the immune system, children must avoid sick contacts, wash hands often, and follow vaccination guidance.
Returning to Normal Life
Most children return to school, play, and regular activities. They may face some restrictions, but life becomes more predictable over time.
Long-Term Outlook for Children After Transplant
Survival Rates Are High
Most children live long, healthy lives after transplant. Improvements in surgery and medications continue to raise survival rates each year.
Possible Long-Term Challenges
Some children face
- Medication side effects
- High blood pressure
- Kidney stress
- Infections
These are monitored regularly.
Quality of Life Is Often Excellent
Most children grow, thrive, and achieve milestones similar to their peers. Many return to sports, travel, and daily routines.
Conclusion
If your child is preparing for a liver transplant, ask your transplant team to walk you through each stage of the journey. Understanding the steps before, during, and after surgery helps reduce fear and builds confidence in the process. Your child’s team is there to support you every step of the way, answer questions, and ensure the safest possible care.
References and Sources
Pediatric Liver Transplant Program at CHOP
Liver Transplant Services at Cincinnati Children’s Hospital