What Is Paediatric Liver Transplant? A Simple Guide for Families Hearing the Word for the First Time

Medicine Made Simple Summary
A paediatric liver transplant is a surgery where a child’s sick liver is replaced with a healthy one from a donor. It is done when the liver can no longer work well enough to keep the child healthy or alive, most often due to childhood liver diseases requiring transplant. The new liver takes over the job of filtering blood, processing nutrients, and fighting infections. Most children who receive a transplant go on to grow, learn, and live more normal lives. Understanding what a liver transplant means helps families prepare for the journey ahead.
Why Families Need a Clear, Simple Explanation
Hearing the words “liver transplant” for the first time can feel overwhelming. Parents often describe the moment as a blur—filled with fear, confusion, and urgent decisions. It is normal to feel uncertain, and many families find it helpful to discuss questions to ask before pediatric liver transplant with their medical team so they can make informed choices. Understanding what a paediatric liver transplant actually is, why it is needed, and how it helps allows families to step into the journey with clarity instead of fear.
This article breaks the topic down into simple, understandable parts so families can follow along even without medical training. Whether you are facing a recent diagnosis or are simply trying to understand the process, this guide offers a foundation to help you feel informed and prepared.
Understanding the Liver: Why It Matters So Much
What the Liver Does in a Child’s Body
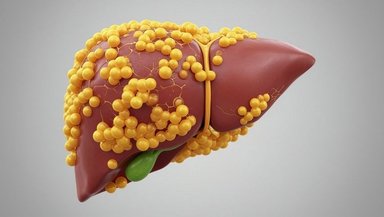
The liver is one of the body’s most important organs. It sits on the right side of the belly and performs hundreds of essential tasks. It removes toxins from the blood, helps digest food, stores energy, builds proteins required for growth, and supports the immune system.
When the liver becomes very sick, these functions slow down or stop. Children may not grow well. Their blood may not clot properly. They may develop jaundice or infections. No machine can fully replace the liver. This is why, when the liver is failing, a transplant becomes the only life-saving option.
Why Children Cannot Survive Without a Working Liver
Some organs—like kidneys—can be supported by machines for long periods. The liver cannot. When the liver stops working, dangerous toxins build up quickly in the bloodstream. Without a transplant, these toxins can affect the brain, heart, and other organs.
A healthy donor liver brings back the functions the child needs to live, grow, and recover.
What Exactly Is a Paediatric Liver Transplant?
A Simple Definition
A paediatric liver transplant is a surgery in which a child’s diseased liver is removed and replaced with a healthy liver or part of a liver from a donor. The new liver takes over immediately, performing all the functions that the damaged liver can no longer manage.
Why Only Part of a Liver Is Sometimes Used
The liver is unique. It can regenerate and grow. This means that a living adult donor can donate a portion of their liver, and both the donor’s remaining liver and the child’s new liver will grow back to normal size over time.
This makes more donor options available for children.
Who Can Be a Donor?
There are three main categories:
- Living relatives or adults who donate a small portion of liver
- Deceased donors
- Split livers, where one donor liver supports two recipients
Each option has benefits depending on urgency, size match, and medical need.
Why Doctors Recommend a Liver Transplant for a Child
When the Liver Cannot Be Saved
Doctors consider a transplant only when the liver is too damaged or diseased to recover. The most common reasons include biliary atresia, metabolic diseases, acute liver failure, and genetic conditions. When medical treatments are no longer enough, transplant becomes the safest and most effective way to save a child’s life.
When Symptoms Show the Liver Is Failing
Several signs show the liver is not functioning well:
- Jaundice that does not improve
- Poor growth
- Frequent infections
- Confusion or irritability
- Fluid buildup in the belly
- Bleeding easily
These symptoms often prompt a transplant evaluation.
The Goal of Transplant
The goal is not only survival. It is also improving the child’s long-term quality of life. Most children who receive a new liver go on to attend school, play sports, eat normally, and meet developmental milestones.
How Doctors Decide Whether a Child Needs a Transplant
Evaluation Is Thorough and Detailed
Before recommending a transplant, doctors perform a complete evaluation. This may take several days or weeks depending on urgency. Tests may include blood work, imaging, heart checks, nutrition assessments, and consultations with multiple specialists.
What Doctors Look For
Doctors determine
- How sick the child is
- Whether the liver can recover
- Whether another treatment option exists
- Whether the child is healthy enough for surgery
- Whether the body can accept a donor liver
This evaluation helps ensure transplant is the right decision.
Understanding the Waiting List
Children needing a deceased donor liver are placed on waiting list. Placement depends on disease severity, age, weight, and urgency. Children with life-threatening liver failure receive priority. Living donor options can shorten waiting time.
What Happens During a Paediatric Liver Transplant Surgery
A Simple Walkthrough of the Procedure
During surgery, the child's diseased liver is removed carefully. The surgeon then connects the donor liver to the child’s blood vessels and bile ducts. These connections allow blood to flow into the new liver and bile to drain properly.
Surgeries often take 6 to 10 hours and involve a large, highly experienced team.
What Makes the Surgery Complex
Children’s livers and blood vessels can be very small. Surgeons must manage bleeding risks, fluid shifts, and delicate anatomy. Because children’s bodies are still growing, the surgical plan is tailored to their size and needs.
How a Child Recovers After the Transplant
The First Days in the ICU
After surgery, children stay in the ICU so the care team can monitor
- Breathing
- Heart rate
- Liver function
- Kidney function
- Fluid balance
The new liver often begins working right away. Some children need ventilator support for a short period.
Immunosuppression Medications Begin
These medications prevent the body from rejecting the new liver. They are essential and must be taken daily. The team adjusts doses as the child grows.
Hospital Stay and Recovery Timeline
Most children stay in the hospital for few weeks. During this time, they begin eating again, start physical therapy, and gradually regain strength.
The Role of the Transplant Team
A Whole-Team Approach to Care
A paediatric liver transplant requires
- Transplant surgeons
- Hepatologists
- Paediatric Intensivist
- Nurses
- Dietitians
- Psychologists
- Pharmacists
- Social workers
- Physical Therapist
This team supports the child’s medical, nutritional, developmental, and emotional needs.
Family-Centered Care
Parents are essential partners. They learn how to manage medications, identify warning signs, and support healing at home.
Long-Term Outlook for Children After Liver Transplant
Survival Rates Are High
Most children survive their transplant and live long, fulfilling lives. Advances in surgery, medications, and paediatric care continue to improve outcomes each year.
Possible Long-Term Challenges
Some children face
- Infections
- Rejection episodes
- Medication side effects
- Growth delays
- Learning difficulties
These are monitored closely with regular follow-ups.
Many Children Live Normal Lives
Most children return to school, play, sports, and everyday routines. They grow, learn, and develop with support from their care teams.
Conclusion
If your child has been advised to undergo a liver transplant, ask your medical team to walk you through the evaluation, donor options, and expected recovery, including the risks of pediatric liver transplant. Understanding the process builds confidence and helps you make informed decisions. You are not alone—your transplant team is there to support you every step of the way.
References and Sources
Paediatric Liver Transplant Program at CHOP
Liver Transplant Services at Cincinnati Children’s