Preparing for Life Post-Transplant: Diet, Vaccines, School, Activities and Long-Term Health After Pediatric Liver Transplant

Made Simple Summary
Life after a pediatric liver transplant involves ongoing care and new daily routines that define life after pediatric liver transplant. Children need a balanced diet, safe vaccination plans, regular school reintegration, thoughtful activity guidelines, and long-term monitoring to protect the new liver. Most children grow stronger over time, return to school, play normally, and live full lives. Parents support recovery by managing medicines, attending follow-up visits, watching for symptoms, and keeping a healthy lifestyle at home. Understanding these long-term steps helps families feel prepared and confident as their child adjusts to life after transplant.
Why Life After Transplant Needs Careful Guidance
A liver transplant gives a child a second chance at life and marks a major milestone in the pediatric liver transplant process. It restores liver function, improves growth, boosts energy, and allows children to return to everyday activities. But while the surgery is a major milestone, it is not the endpoint. Life after transplant brings a new rhythm—one that balances freedom with responsibility.
Parents often ask: What should my child eat? When can they return to school? Are vaccines safe? When can they exercise again? How do we protect the new liver? This guide answers these questions in simple, direct language so families can understand what life looks like after transplant.
Life after transplant can be joyful and full, but it requires careful planning, consistent routines, and close follow-up with the medical team, often coordinated through choosing a pediatric liver transplant center with strong long-term care programs.
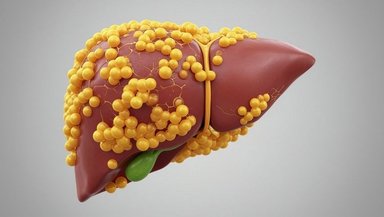
Diet and Nutrition After Liver Transplant
Why Nutrition Plays a Key Role in Recovery Term Health After Pediatric Liver Transplant
Medicine
Good nutrition helps the body heal, strengthens the immune system, and supports healthy growth. After transplant, many children experience increased appetite, better digestion, and improved energy. Others may need extra help rebuilding muscle or regaining weight.
The nutrition team guides parents through each phase.
What Your Child Can Eat After Transplant
Most children return to regular eating fairly quickly, but the diet must be safe and well-balanced. The main goals are
Adequate calories for healing
Enough protein for muscle repair
Healthy fats for growth
Vitamins and minerals for metabolic balance
Parents can gradually reintroduce their child’s usual foods as tolerated. Eating becomes easier as the new liver begins functioning well.
Foods to Avoid in the Early Period
During the first months, certain foods increase the risk of infection or foodborne illness. These include
Raw or undercooked eggs
Unpasteurized dairy
Raw fish or shellfish
Deli meats not reheated
Buffet foods that may not be temperature-safe
Safe food practices protect the new liver and the immune system.
Hydration and Salt Intake
Good hydration reduces kidney stress, especially because some medicines affect kidney function. Doctors may recommend limiting salt if blood pressure rises.
Vitamin and Mineral Support
Some children need supplements such as
Vitamin D
Calcium
Magnesium
Iron
These support bone health, immune strength, and red blood cell production.
Weight and Appetite Changes
Immunosuppressants may increase appetite. Parents should encourage healthy choices and avoid excessive sugary foods. A dietitian can help manage weight changes if needed.
Vaccines After Liver Transplant
Why Vaccination Rules Change After Transplant
Before transplant, children often receive catch-up vaccines. After transplant, the immune system becomes weaker due to immunosuppressants. This changes which vaccines are safe.
What Vaccines Are Safe After Transplant
Most inactivated vaccines are safe and recommended. These include
Influenza
Pneumococcal
Diphtheria, tetanus, pertussis
Polio (inactivated form)
Hepatitis A and B
These vaccines protect against infections that may be more serious for transplant recipients.
Vaccines That Are Not Safe Immediately After Transplant
Live vaccines are usually not given right away. These include
MMR
Varicella
Rotavirus
Some children may safely receive certain live vaccines later, but only under strict guidance.
Talking With the Transplant Team Before Any Vaccine
Parents should always check with their team before giving any vaccine. Timing matters. Some vaccines are delayed for months until the child’s immune system stabilizes.
Returning to School After Liver Transplant
When Most Children Return to School
Many children return to school within six months after transplant. Some may need a longer recovery period. The team considers
Immune status
Appetite and strength
Psychological readiness
Seasonal infection risk
A return-to-school plan should be individualized.
Preparing Teachers and School Staff
Parents should inform the school about
Medication times
Infection precautions
Activity restrictions
Emergency contacts
Any accommodations needed
A school nurse or teacher familiar with medical needs helps ensure a smooth transition.
Protecting Against Infections at School
Children must avoid close contact with sick classmates, especially in the early months. Teachers can help by encouraging
Handwashing
Clean classrooms
Notifying parents of illness outbreaks
Masks may be recommended in certain seasons or during outbreaks.
Emotional Transition Back to School
Some children feel excited. Others feel nervous or overwhelmed. They may worry about falling behind or being asked questions about their transplant. Child-life specialists and counselors can help prepare them emotionally.
Physical Activity and Play After Transplant
Why Movement Matters
Physical activity improves strength, mood, bone health, and overall confidence. Movement also supports recovery by improving blood flow and reducing stiffness.
When Activity Can Resume
Activity resumes gradually. The general pattern looks like this:
Weeks 1–6: Gentle walking, light play
Weeks 6–12: More active play, gradual increase in endurance
After 12 weeks: Most non-contact activities resume
Each child progresses differently. The surgical incision must heal fully before strenuous movement.
Activities to Avoid Initially
Avoid activities that risk abdominal injury. These include
Football
Martial arts
Gymnastics with flips
Heavy lifting
Trampolines
Such activities may return later depending on recovery.
Encouraging Confidence Through Movement
Children may fear pain or feel unsure about using their bodies again. Parents can encourage small steps, celebrate progress, and work with physical therapists when needed.
Long-Term Medications and Health Monitoring
Lifelong Immunosuppressants
Children must take immunosuppressants daily. These prevent the body from rejecting the new liver. Medication doses adjust as children grow.
Missing doses increases the risk of rejection. Families should use alarms, pill boxes, or reminders to stay on schedule.
Long-Term Follow-Up Visits
Children require lifelong follow-up. The schedule usually looks like
Weekly or biweekly visits early
Monthly visits in coming months
Every few months in later years
Annual visits in stable adolescence and adulthood
Blood tests monitor
Liver enzymes
Kidney function
Medication levels
Infection markers
Follow-up is essential, even when the child feels healthy.
Monitoring for Long-Term Risks
Possible long-term risks include
High blood pressure
High blood sugar
Kidney strain
Bone weakness
Weight changes
Infections
These risks are manageable when caught early.
Mental and Emotional Health After Transplant
Why Emotional Recovery Takes Time
Children may experience
Fear of future illness
Worry about medical visits
Frustration with limitations
Sadness about missing school or activities
Parents should watch for signs of anxiety or depression and seek help when needed.
How to Support Emotional Healing
Encourage open conversations
Provide predictable routines
Reinforce the child’s strengths
Celebrate milestones
Involve child-life specialists or therapists
Emotional resilience grows when children feel understood and supported.
Helping Teenagers Understand Their Health
Teens must eventually take responsibility for
Medicines
Appointments
Recognizing symptoms
Healthy lifestyle choices
Preparing them early builds independence.
Family Life After Transplant
Adjusting to New Routines
The family may need to adjust schedules around medicines, follow-ups, or school needs. Over time, these routines become part of daily life.
Supporting Siblings
Siblings may feel left out or worried. Including them in age-appropriate ways helps maintain family balance.
Returning to Normal Life
Most families return to normal routines within months. Travel, social events, and sports become possible again with medical guidance.
Long-Term Outlook for Children After Liver Transplant
Most Children Thrive
Children often experience improved growth, better energy, stronger immunity, and a higher quality of life. Many participate in sports, excel in school, and enjoy regular childhood experiences.
Transplant Is a Partnership for Life
Parents, children, and the transplant team work together for years. With consistent care, most children enjoy excellent long-term outcomes.
Conclusion
If your child has had a liver transplant or is preparing for one, talk to your transplant team about long-term care, diet guidelines, vaccines, school planning, and activity safety. With the right guidance, your child can return to a full and healthy life. You are not alone in this journey—your team is there to support you every step of the way.
References and Sources
Pediatric Liver Transplant Program – CHOP
Liver Transplant Services – Cincinnati Children’s