Living Donor vs Deceased Donor vs Split Liver Transplant — What Are Your Child’s Options?

Medicine Made Simple Summary
Children who need a liver transplant often develop advanced liver damage due to childhood liver diseases requiring transplant, and they can receive a liver from a living donor, a deceased donor, or through a split liver transplant. A living donor gives a small part of their liver, which grows back in both donor and child. A deceased donor liver comes from someone who has passed away and donated their organs. A split liver transplant divides one donor liver to help two people. Each option has benefits, challenges, and different wait times. Understanding these choices helps families make confident decisions.
Why Families Need Clear Information About Donor Types
When parents hear that their child needs a liver transplant, one of the first questions they ask is, “Where will the new liver come from?” Understanding donor options is essential. Each type—living donor, deceased donor, and split liver—has unique advantages, risks, and timelines. Some options offer faster surgery. Others depend on organ availability. Knowing these choices early helps families prepare emotionally and medically for the transplant journey.
This article explains each donor option in simple, clear language so families can feel informed, confident, and prepared.
Why Donor Type Matters in Pediatric Liver Transplant
The Liver’s Unique Ability to Regrow
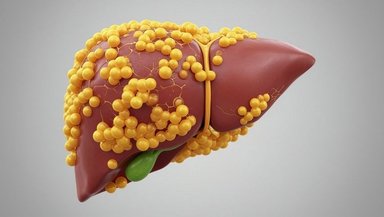
Unlike most organs, the liver can regenerate. This remarkable feature makes living donor and split liver transplants possible. Both the donor and the child can regrow a full liver from a partial graft. This means children are not limited only to deceased donors and may have more options for matching.
Why Children Benefit from More Donor Choices
Children often become very sick while waiting for a transplant. Their small size makes finding a perfect match harder. Having more donor options increases the chance of getting a transplant sooner, which can significantly improve outcomes.
Three Donor Types Explained Simply
Living donor liver transplant
Deceased donor liver transplant
Split liver transplant
Each option has its own process, timeline, and benefits. Understanding these differences is the first step toward making an informed decision.
1. Living Donor Liver Transplant
What Is a Living Donor Liver Transplant?
A living donor transplant uses a portion of a healthy adult's liver—usually a parent, relative, or volunteer—to replace the sick liver in a child. The donor’s remaining liver grows back to normal size. The child’s transplanted portion also grows and functions like a full liver.
Who Can Be a Living Donor?
Donors must be healthy adults with compatible blood types, appropriate liver size, and no medical conditions that increase risk. Most donors are family members because they share genetics and often have matching blood groups. Some centers allow unrelated donors if they meet medical and psychological criteria, which is why families are encouraged to discuss questions to ask before pediatric liver transplant in detail with the transplant team.
Why Living Donor Transplants Are Often the Best Option for Children
Shorter waiting time
Better control over timing of surgery
Better outcomes for many infants with biliary atresia
Lower risk of complications in certain conditions
Faster recovery
Because timing is predictable, the child can undergo transplant before becoming critically ill.
Risks for the Donor
Living donation is major surgery. Risks include
Pain
Bleeding
Infection
Bile leaks
Long-term outcomes for donors are excellent, and the liver typically regrows completely within months. Donor safety is the top priority.
Risks for the Child
The child may experience
Rejection
Infection
Bile duct problems
These risks exist regardless of donor type.
When Living Donation Is Not Possible
If the donor is medically unsuitable
If blood types do not match
If the liver size or anatomy is not compatible
If the child’s condition requires urgent deceased donor transplant
2. Deceased Donor Liver Transplant
What Is a Deceased Donor Transplant?
A deceased donor liver comes from someone who has passed away and previously chosen to donate their organs. These organs are carefully matched to children based on blood type, size, urgency, and medical need.
How Children Receive Deceased Donor Livers
Children are placed on a national waiting list
Priority is based on how sick the child is
Smaller children receive organs from pediatric or small adult donors
Placement on the list does not mean an exact time for transplant. Families often wait days, weeks, or months depending on availability.
Benefits of Deceased Donor Transplants
No family member undergoes surgery
Larger livers may be available for older children
Often used for urgent, unexpected liver failure
Suitable when living donor is not an option
Challenges With Deceased Donation
Waiting times can be unpredictable
Sicker children may need transplant sooner than organs become available
The child may become unstable during the wait
Families must stay ready to come to the hospital as soon as an organ becomes available.
3. Split Liver Transplant
What Is a Split Liver Transplant?
A split liver transplant divides a deceased donor liver into two parts so it can save two people. Typically, the smaller left lobe goes to a child and the larger right lobe goes to an adult. Because children need only a small graft, this option increases the number of available organs.
Why Split Liver Transplants Are Important for Children
More donor organs become available
Children receive priority because their portion is smaller
Outcomes in experienced centers are excellent
This option is especially useful for infants and young children.
Limitations of Split Transplants
Not every liver can be split
The donor must be healthy and size-appropriate
Transplant centers must have expertise to perform the procedure safely
Some cases still require whole livers
Suitability for Each Child
Doctors determine whether a split graft is appropriate based on the child’s size, condition, and urgency.
Comparing the Three Donor Options
Below is a simple, clear comparison to help families understand the differences.
Living Donor Transplant
Predictable timing
Often quicker
Donor must be healthy
Surgery for both donor and child
Deceased Donor Transplant
No surgery for donor
Wait time unpredictable
Used in emergencies
Dependent on organ availability
Split Liver Transplant
One donor helps two recipients
Often prioritized for children
Requires special surgical expertise
Not always possible
How Doctors Decide Which Donor Option Is Best
Medical Condition and Urgency
Children with sudden liver failure may need the fastest option available—often a deceased donor. Children with long-term disease like biliary atresia may do well with a planned living donor transplant.
Size and Blood Type Matching
Doctors match donors and children based on size, blood type, and anatomy. Small babies require very small grafts.
Liver Anatomy
Some donors have anatomical variations that make them unsuitable for splitting or for living donation.
Center Expertise
Not all centers perform living donor or split liver transplants. Centers with these capabilities offer more flexibility.
Which Option Has the Best Outcomes?
Living Donor Transplants Have Excellent Outcomes
Children often experience
Shorter waiting times
Fewer complications
Better survival rates in certain diseases
Deceased Donor Survival Is Also High
Deceased donor organs work well and are life-saving, especially in emergencies.
Split Liver Survival Is Similar When Performed at Experienced Centers
Studies show that outcomes are comparable to whole liver transplants when performed by specialized teams.
What Parents Should Consider Before Making a Decision
Health and Willingness of a Potential Donor
A willing donor must be medically suitable. Some parents, relatives, or family friends volunteer but may not meet criteria. This is normal and should not cause guilt.
Waiting List Risks
If the child is becoming very sick, waiting may be unsafe. Living donation may offer a faster solution.
Logistics of Donor and Child Surgery
Families must consider time off work, caregiving for siblings, and transportation during recovery.
Long-Term Care After Transplant
Regardless of donor type, the child will need
Lifelong follow-up
Immunosuppression medications
Regular labs
The donor type does not change long-term medication needs.
Conclusion
If your child is being considered for a liver transplant, ask your transplant team which donor options are available and why one may be better than another. Understanding these choices early helps you plan, ask informed questions, and feel confident in the path ahead. Your medical team will guide you through every step and support your family’s decisions.
References and Sources
Pediatric Liver Transplant Program – CHOP
Liver Care – Nationwide Children’s Hospital
Pediatric Liver Transplant – UCSF Benioff Children’s Hospital