Pleural Fluid: What Causes It, Symptoms to Watch For, and When to See a Doctor
Medicine Made Simple Summary
When excess fluid collects around the lungs, doctors may need to remove it using a simple medical procedure called thoracentesis. This procedure involves inserting a thin needle into the chest to drain the fluid safely. It helps patients breathe better and allows doctors to test the fluid to find the cause. Thoracentesis is usually done under local anesthesia, does not require surgery, and often provides quick relief.
Understanding why this procedure is done and how it fits into care helps patients and families feel calmer and better prepared.
What Pleural Fluid Is and Why the Body Needs It
The lungs are surrounded by a thin lining called the pleura. One layer of this lining covers the lungs, and the other lines the inside of the chest wall. Between these two layers is a very small space that contains pleural fluid.
This fluid has an important role. It allows the lungs to slide smoothly as we breathe. Without it, every breath would cause friction and discomfort. In healthy people, the amount of pleural fluid is very small and carefully balanced.
Problems begin when this balance is disturbed and fluid starts to accumulate.
When Pleural Fluid Becomes a Medical Problem
When excess pleural fluid builds up, the condition is called pleural effusion. The extra fluid presses on the lungs from the outside. This limits how much the lungs can expand and makes breathing harder.
Pleural effusion is not a disease by itself. It is a sign that something else in the body is causing fluid imbalance, inflammation, or blockage of normal drainage pathways. Understanding this helps patients realize why doctors focus on finding the cause, not just removing the fluid.
Why Doctors Sometimes Need to Remove Pleural Fluid
Doctors consider removing pleural fluid when it affects breathing or when the cause is unclear. Excess fluid can make even simple activities like walking or talking feel exhausting.
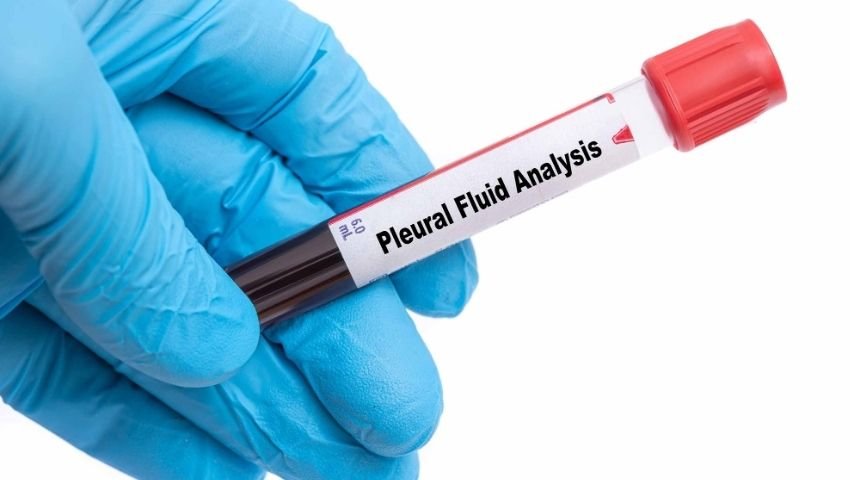
Removing the fluid relieves pressure on the lungs and improves comfort. At the same time, the fluid can be sent to a laboratory for testing. This testing helps doctors identify infections, cancer, inflammation, or problems related to the heart, liver, or kidneys.
This is where thoracentesis becomes important.
How Thoracentesis Fits Into Pleural Fluid Management
Thoracentesis is the procedure doctors use to remove pleural fluid. It is not surgery and does not involve large cuts. A thin needle or small tube is inserted through the chest wall into the fluid-filled space.
The procedure is usually done while the patient is awake. Local anesthesia numbs the area, making the procedure more comfortable. Thoracentesis can remove small or large amounts of fluid, depending on the situation.
For many patients, breathing becomes easier soon after the fluid is removed.
Common Causes of Excess Pleural Fluid
Pleural fluid can build up for many reasons. Heart failure is one of the most common causes. When the heart cannot pump effectively, fluid backs up into the lungs and surrounding tissues.
Lung infections like pneumonia cause inflammation, allowing fluid to leak into the pleural space. Kidney and liver diseases disrupt the body’s ability to manage fluids properly.
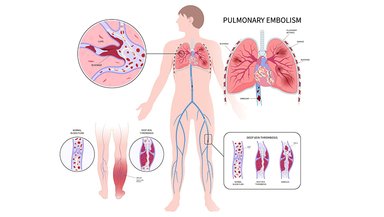
Cancer can cause pleural fluid buildup by irritating the pleura or blocking fluid drainage. Blood clots in the lungs, chest injuries, autoimmune diseases, and post-surgical inflammation can also lead to pleural effusion.
Sometimes, the cause is not immediately obvious, which is why fluid analysis becomes important.
Symptoms That Suggest Pleural Fluid Buildup
Shortness of breath is the most common symptom. Many patients notice that breathing becomes harder when lying flat. Chest pain may occur, especially with deep breaths or coughing.
A dry cough, fatigue, and chest heaviness are also common. Some patients may not have symptoms if the fluid buildup is small or slow.
Any unexplained breathing difficulty should be evaluated by a doctor.
How Doctors Detect Pleural Fluid
Doctors often suspect pleural fluid based on symptoms and physical examination. Reduced breath sounds on one side of the chest can be a clue.
Imaging tests confirm the diagnosis. Chest X-rays show larger fluid collections. Ultrasound can detect smaller amounts and guide fluid removal. CT scans provide detailed views when needed.
Once fluid is confirmed, doctors decide whether monitoring or intervention is required.
Why Fluid Testing Is Important
Removing pleural fluid is not just about symptom relief. The fluid itself carries valuable information. Laboratory testing can reveal infection, cancer cells, inflammation, or fluid imbalance.
These results guide treatment decisions. For example, infections require antibiotics, while cancer-related effusions may need specialized care.
Without fluid testing, treatment may be delayed or incomplete.
When Pleural Fluid Does Not Need Immediate Removal
Not all pleural fluid requires thoracentesis. Small amounts that cause no symptoms may be monitored closely.
Doctors consider factors such as breathing difficulty, overall health, and suspected cause before recommending fluid removal. Monitoring may involve repeat scans and clinical follow-up.
This careful approach avoids unnecessary procedures while keeping patient safety first.
What Happens If Pleural Fluid Keeps Returning
In some patients, pleural fluid returns even after removal. This is more common in chronic conditions like heart failure or certain cancers.
Repeated thoracentesis may be needed in some cases. In others, long-term solutions may be discussed. The goal is always to balance comfort, safety, and quality of life.
Understanding this helps patients prepare for long-term management if needed.
Emotional Impact of Pleural Fluid Diagnosis
Being told there is fluid around the lungs can cause fear and uncertainty. Many patients worry about serious illness or permanent lung damage.
Clear explanations help reduce anxiety. Knowing that pleural fluid is common and often treatable brings reassurance. Understanding why procedures like thoracentesis are done helps patients feel more in control.
Family support plays a key role during this time.
Why Awareness and Early Care Matter
Ignoring early symptoms can lead to worsening breathing problems and complications. Early evaluation allows doctors to identify pleural fluid before it becomes severe.
Timely treatment improves comfort and outcomes. Education empowers patients to seek care without delay.
Conclusion
If you or a loved one experiences unexplained breathlessness, chest pain, or persistent cough, consult a doctor promptly. Early evaluation can identify pleural fluid and determine whether procedures like thoracentesis are needed. Understanding the process helps you take an active role in your care.