How to Prepare for Thoracentesis: Questions to Ask Before Your Procedure

Medicine Made Simple Summary
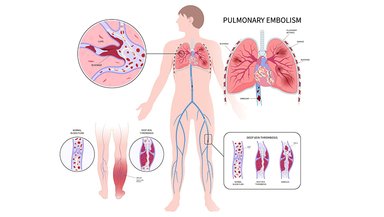
Thoracentesis is a procedure used to remove fluid from around the lungs to improve breathing and find the cause of the fluid buildup. Preparing for thoracentesis mainly involves understanding why it is needed, knowing what will happen during the procedure, and asking the right questions beforehand. Most patients do not need major preparation, but clear communication with the doctor helps reduce fear and prevents surprises. Knowing what to expect before, during, and after thoracentesis helps patients and families feel calmer and more confident.
Why Preparation Matters Even for a Simple Procedure
Thoracentesis is usually a straightforward and safe procedure, but it still involves the chest and breathing. This naturally makes people anxious. Preparation is not about complicated steps or strict rules. It is about mental readiness, understanding the purpose of the procedure, and ensuring safety.
Patients who understand why thoracentesis is recommended often feel less fear. Families who know what to expect are better able to provide support. Preparation turns an unfamiliar medical experience into a manageable one.
Understanding Why Thoracentesis Is Being Done
Before the procedure, it is important to know why thoracentesis has been advised. Doctors may recommend it to relieve breathlessness, to test the fluid, or for both reasons.
Some patients assume thoracentesis is always urgent or dangerous. In reality, it is often planned carefully after imaging shows fluid around the lungs. Understanding the reason helps patients appreciate the benefits and reduces unnecessary worry.
What Information to Share With Your Doctor
One of the most important parts of preparation is sharing accurate information. Patients should tell their doctor about any medicines they take, especially blood thinners. These medicines may increase the risk of bleeding and sometimes need adjustment.
Allergies, especially to local anesthetics or antiseptics, should be mentioned. Any history of lung disease, previous chest procedures, or bleeding disorders is also important.
Honest communication helps doctors plan the procedure safely.
Do You Need to Stop Eating or Drinking
Most thoracentesis procedures do not require fasting. Patients are usually allowed to eat and drink normally unless told otherwise. This surprises many people who expect strict instructions.
If thoracentesis is planned along with another procedure or imaging study, special instructions may apply. Always follow the specific advice given by the healthcare team.
Clothing and Personal Preparation
On the day of thoracentesis, patients are usually asked to wear a hospital gown. Comfortable clothing makes changing easier. Jewelry around the chest or neck area should be removed.
Patients should arrange for someone to accompany them if possible, especially if they feel anxious or weak. While many people can go home on their own, emotional support is helpful.
What to Expect When You Arrive
When patients arrive for thoracentesis, vital signs such as blood pressure, pulse, and oxygen levels are checked. Imaging tests like ultrasound may be repeated to confirm the fluid location.
The doctor explains the procedure again and answers last-minute questions. This is a good time to speak up about fears or discomfort.
Knowing these steps in advance helps reduce stress.
Key Questions to Ask Before Thoracentesis
Patients should feel comfortable asking questions. Important questions include why thoracentesis is needed, how much fluid will be removed, and whether the fluid will be tested.
Other useful questions involve pain control, possible risks, and what symptoms to watch for afterward. Patients may also ask how long the procedure takes and whether they can go home the same day.
Asking questions is not a sign of doubt. It is a sign of active participation in care.
How Doctors Prepare for Safety
Doctors take several precautions before thoracentesis. Imaging helps locate the safest spot for fluid removal. Ultrasound guidance is often used to reduce complications.
The skin is cleaned carefully to prevent infection. Local anesthesia is prepared to numb the area. Monitoring equipment is readied to track breathing and oxygen levels.
These steps are routine and designed to keep patients safe.
Mental Preparation and Managing Anxiety
Fear before thoracentesis is common. Patients worry about pain, breathing problems, or complications. Talking openly with the doctor can ease many of these fears.
Deep breathing, relaxation techniques, and reassurance from family members can help. Understanding that thoracentesis is commonly performed and usually well tolerated reduces anxiety.
Mental preparation is just as important as physical preparation.
What Happens Immediately Before the Procedure
Just before thoracentesis, patients are positioned carefully, usually sitting upright or leaning slightly forward. The skin is cleaned, and the numbing medicine is injected.
Patients may feel a brief sting from the anesthetic. After that, the area becomes numb. The doctor explains each step as it happens.
Knowing this sequence in advance helps patients remain calm.
Preparing for After the Procedure
Preparation also includes knowing what happens afterward. Patients should ask how long they will be observed and whether a chest X-ray will be done.
Mild soreness at the needle site is common. Patients should ask when they can resume normal activities and which symptoms require medical attention.
Planning for rest after the procedure is helpful.
Role of Family Members in Preparation
Family members play an important role. They help patients remember instructions, ask questions, and provide emotional support.
Having a trusted person present can reduce anxiety and improve understanding. Families should also understand the purpose of thoracentesis so they can offer reassurance.
Common Myths About Preparation
Some people believe thoracentesis requires strict fasting or heavy sedation. Others think it always requires hospital admission. These beliefs are usually incorrect.
Thoracentesis is often done with local anesthesia and minimal preparation. Clarifying myths helps patients approach the procedure with realistic expectations.
Why Being Informed Makes a Difference
Patients who are informed tend to feel more in control. They are more likely to report symptoms early and follow instructions correctly.
Preparation improves the overall experience and builds trust between patients and healthcare providers.
Conclusion
If thoracentesis has been recommended, take time to discuss it with your doctor. Ask questions, share your medical history, and clarify instructions. Being prepared helps you approach the procedure calmly and confidently, making the experience safer and less stressful.
References and Sources
Cleveland Clinic – Thoracentesis: What to Expect
RadiologyInfo.org – Thoracentesis Patient Guide