“When you feel like quitting, think about why you started.”
Morbid Obesity or clinically severe Obesity has emerged as one of the most dreaded diseases of this century. People who have attempted to lose weight, know how difficult it is to not only lose weight but also to maintain the weight loss. Daily, we see patients who put their heart and soul into their efforts to lose weight. They have been to every weight loss clinic, celebrity dietician, gym, yoga guru and weight loss retreat. Unfortunately, more often than not, they meet with disappointment and tend to yo-yo between weight loss and weight gain. This entire process is extremely disheartening and demotivating.
So, if you have tried hard to lose weight without success and the weight is bearing you down, you have come to the right place because Bariatric surgery is the only way at the moment that can lead to sustained weight loss in morbidly obese patients.
Laparoscopic Sleeve Gastrectomy
Laparoscopic Sleeve Gastrectomy is one of the most popular weight loss Bariatric procedures. It was first performed in the United States of America in the 1990s as a part of the Duodenal Switch Surgery. It is a technically simpler and easier procedure to perform and has shown good weight loss results.
Am I the right candidate for undergoing Laparoscopic Sleeve Gastrectomy
The IFSO - APC (International Federation for Surgery for Obesity and Metabolic Disorders - Asia Pacific Chapter) guidelines for weight loss surgery are as under:
- Bariatric surgery/Obesity surgery/weight loss surgery must be considered for the treatment of Obesity for acceptable Asian candidates with BMI ≥ 35 Kg/m2 with or without any associated diseases.
- Bariatric surgery/metabolic surgery must be considered for the treatment of type 2 diabetes or metabolic syndrome for patients who are inadequately controlled by lifestyle alterations and medical treatment for acceptable Asian candidates with BMI ≥ 30 Kg/m2.
- Bariatric surgery/metabolic surgery may also be considered as a non-primary alternative to treat inadequately controlled type 2 diabetes or metabolic syndrome for suitable Asian candidates with BMI ≥ 27.5 Kg/m2.
Laparoscopic Sleeve Gastrectomy is usually preferred in younger patients, with a shorter duration of type 2 diabetes, and not too many associated co-morbidities.
It is also performed as a first-stage surgery in obese patients. A sleeve gastrectomy can easily be converted into other Bariatric and metabolic procedures such as Roux-en-Y Gastric Bypass, Duodenal Switch, SADI-S, Duodeno-jejunal Bypass and Ileal Transposition.
It must not be performed in patients suffering from acid reflux disease and hiatus hernia.
How is it done?
- As the name suggests, this surgery is performed by Laparoscopic technique. In this technique, 4 to 5 tiny 0.5 to 1 cm cuts are made on your tummy and the entire surgery is performed using a camera and instruments. This is minimally invasive and there is no big cut like the surgeries of the past. All the stitches are absorbable and no sutures are to be removed later. Laparoscopy enables the patient to have less pain, recover faster and return to work much earlier. Most patients are discharged from the hospital one day after their operation. Of course, this depends on their clinical status as well.
- Single incision sleeve gastrectomy: In this technique, a 2 cm cut is made in the navel and the entire surgery is performed through this cut. Once this heals, the scar gets deeply buried in the navel and it is practically scarless. It is less painful and gives the patient the benefit of confidentiality. It is quite popular amongst young, unmarried women.
- During the surgery, a vertical sleeve of the Stomach is created over a 38 French bougie using surgical staplers. The remaining part of the Stomach is removed from the body.
How does it lead to weight-loss
The following mechanisms lead to weight loss after Laparoscopic Roux-en Y Gastric Bypass.
- A small Stomach pouch restricts the amount of food that a person can eat. There is significant caloric restriction after this surgery.
- After this surgery, the Stomach empties at a faster rate and this leads to activation of certain Intestinal hormones which aid in weight loss as well as remission of co-morbidities such as Type 2 Diabetes etc.
- There are many other mechanisms and yet unidentified roles of bile acids and gut flora that may help in weight loss and remission of co-morbidities after this surgery.
Results of Laparoscopic Sleeve Gastrectomy
- Patients lose up to 65 to 75% of their excess weight throughout 12 to 18 months after this surgery. This can be even better if the patient embraces lifestyle modification and follows a strict diet and exercise program as guided by the Bariatric surgery team.
- This surgery also leads to a significant improvement in associated diseases such as type 2 diabetes, high blood pressure, high cholesterol, heart disease, risk of venous thromboembolism, gout and so on.
Long-term weight loss goals
- Bariatric surgery must not be perceived as a shortcut to weight loss. The patient and the doctor work as a team to achieve the best results in the long term. It is extremely important to be diligent with your follow-up to get optimum results.
- Long-term weight loss goals can be achieved with the help of a team that consists of a doctor, an endocrinologist, a nutritionist and a psychologist. This support team of experts will keep you motivated, provide advice and help you to work through weight-loss barriers.
Who is not eligible for weight loss surgery
- Pregnant women
- Patient with acid reflux disease and hiatus hernia
- Patient with gastric outlet obstruction
- Patients with severe psychiatric disorders
- Smokers
- Patients with the inability to take nutritional supplements
- Patients who are medically unfit for surgery and Anaesthesia
Complications
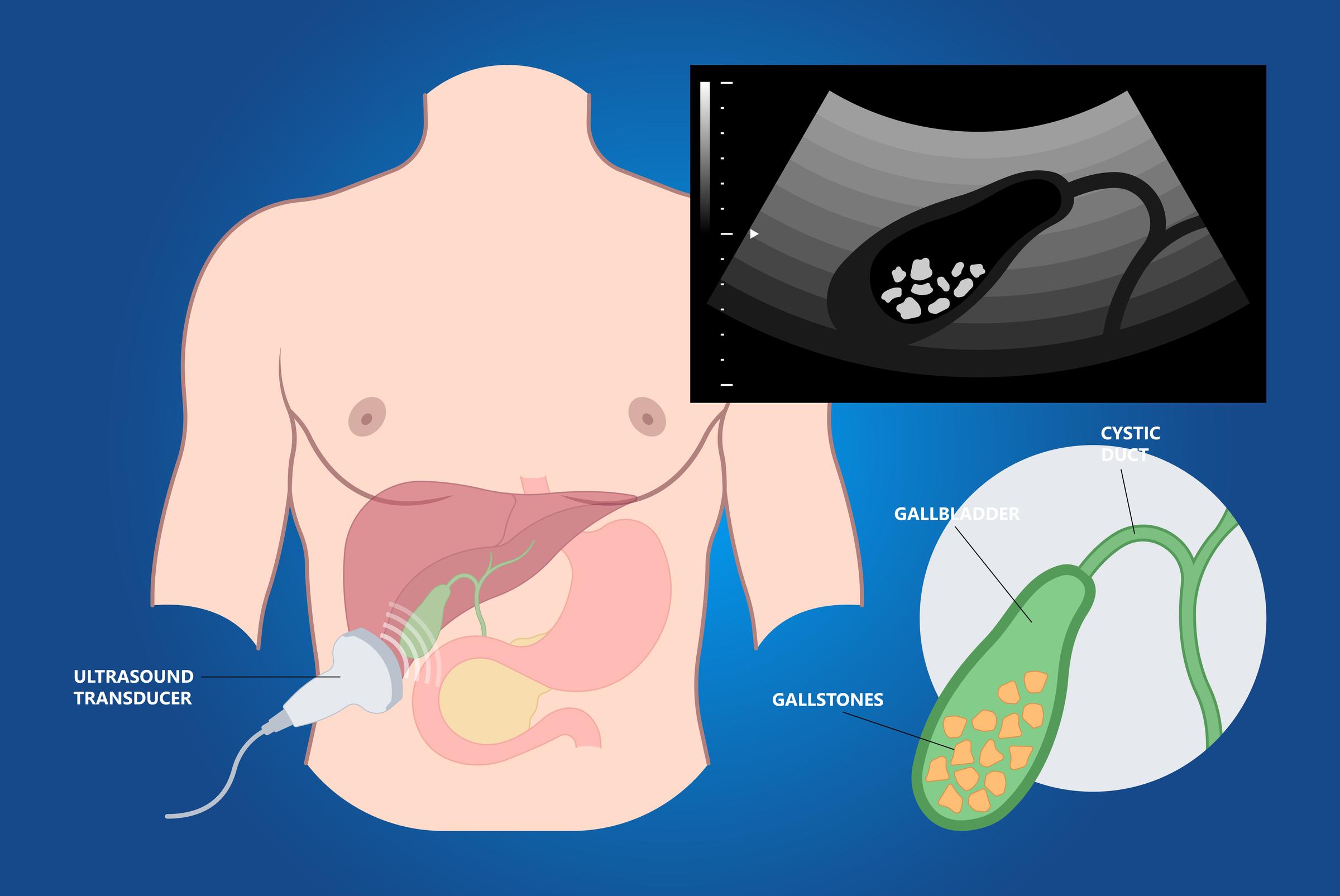
- Laparoscopic Sleeve Gastrectomy is as safe as any other surgery like a knee replacement or a gall bladder surgery. The complication rate is much lower than Cancer surgery or surgery for the esophagus, valve replacement etc.
- It is important to follow the protocols set by the team and to take nutritional supplements as advised. Failure to do so may result in nutritional deficiencies in future.
- Smokers must strictly stop smoking. Smoking can lead to complications that can be life-threatening. If you are not confident about giving up smoking after this surgery, our advice is that you must not undergo the surgery at all.
- The team will discuss the pros and cons in detail with you during your consultation.
Dr Aparna Govil Bhasker has one of the highest experiences in performing Laparoscopic as well as single incision sleeve gastrectomy in the country. She believes in quality care and will make it extremely safe for you. You will be in good hands so do not worry. The biggest plus of coming to us for your surgery is our personalized care. Every patient is a VIP for us and we assure you that your smallest queries will be addressed at the earliest.
The patient needs to be mentally prepared and in a positive frame of mind before undergoing any kind of surgery. Positive thoughts go a long way in getting good results after surgery. So, be positive and we wish you all the best for your weight-loss journey to being a different you.