1. Induction:
- The process of inducing general anesthesia begins in the pre-operative area or operating room. Patients are usually asked to breathe in anesthetic gases through a mask or receive medication intravenously to initiate the anesthesia process.
- The induction phase aims to transition the patient from a conscious state to unconsciousness smoothly and rapidly.
2. Maintenance:
- Once the patient is unconscious, the anesthesia is maintained throughout the surgery. Anesthesia providers continuously monitor the patient's vital signs, including heart rate, blood pressure, oxygen saturation, and breathing, to ensure their safety and adjust the anesthesia levels as needed.
- During this phase, additional medications may be administered to maintain the desired depth of anesthesia and to control pain and muscle relaxation.
3. Airway Management:
- Maintaining a patent airway is crucial during general anesthesia to ensure adequate oxygenation and ventilation.
- Anesthesia providers may utilize techniques such as endotracheal intubation (insertion of a breathing tube into the trachea) or a supraglottic airway device to secure the airway and facilitate mechanical ventilation.
4. Muscle Relaxation:
- General anesthesia often involves the use of muscle relaxants to induce temporary paralysis of skeletal muscles. This paralysis allows the surgical team to perform procedures more safely by preventing involuntary movements and optimizing surgical conditions.
- Anesthesia providers carefully titrate the muscle relaxants to achieve the desired level of paralysis while minimizing side effects.
5. Monitoring:
- Throughout the surgical procedure, patients under general anesthesia are continuously monitored to ensure their safety and well-being.
- Monitoring typically includes electrocardiography (ECG) to assess heart function, pulse oximetry to measure oxygen saturation in the blood, capnography to monitor carbon dioxide levels in exhaled breath, and blood pressure monitoring.
6. Emergence and Recovery:
- As the surgical procedure nears completion, anesthesia delivery is gradually reduced to allow the patient to emerge from the unconscious state.
- After surgery, patients are transferred to the post-anesthesia care unit (PACU), where they are closely monitored during the recovery process.
- Anesthesia providers manage the transition from unconsciousness to consciousness and address any post-operative pain or nausea to ensure a smooth recovery.
General anesthesia is a complex medical intervention that requires careful monitoring, precise dosing of medications, and skilled management by trained anesthesia providers. While it carries inherent risks, advancements in anesthesia techniques and monitoring equipment have significantly improved patient safety and outcomes during surgery.
General anesthesia is a type of anesthesia that induces a reversible loss of consciousness and sensation throughout the entire body. It is commonly used for major surgeries or procedures that require the patient to be completely unconscious. During general anesthesia, the patient's vital signs, including heart rate, blood pressure, and oxygen levels, are closely monitored to ensure safety and optimal outcomes.
1. Types of Regional Anesthesia:
- Epidural Anesthesia: Involves injecting anesthetic medication into the epidural space surrounding the spinal cord. This technique provides pain relief for procedures such as childbirth, lower abdominal surgeries, and lower limb surgeries.
- Spinal Anesthesia: Similar to epidural anesthesia but involves injecting the anesthetic medication directly into the cerebrospinal fluid surrounding the spinal cord. Spinal anesthesia results in rapid onset and more profound anesthesia, making it suitable for procedures like cesarean sections, lower limb surgeries, and urological surgeries.
- Peripheral Nerve Blocks: Target specific nerves to numb a particular area of the body. Peripheral nerve blocks are commonly used for surgeries involving the extremities, such as orthopedic procedures, hand surgeries, and foot surgeries.
2. Mechanism of Action:
- Regional anesthesia works by blocking nerve impulses in the targeted area, preventing the transmission of pain signals to the brain.
- Local anesthetic medications, such as lidocaine or bupivacaine, are injected near the nerves or nerve roots responsible for sensation in the region undergoing surgery.
- The onset and duration of regional anesthesia depend on factors such as the type and concentration of the local anesthetic used, as well as the specific technique employed by the anesthesia provider.
3. Administration:
- Regional anesthesia is typically administered by an anesthesia provider, such as an anesthesiologist or nurse anesthetist, who has specialized training in nerve block techniques.
- The procedure may involve using ultrasound guidance to precisely locate the nerves and administer the local anesthetic medication with accuracy.
- Patients may receive sedation to help them relax during the procedure, although they remain conscious and able to communicate with the anesthesia provider.
4. Benefits:
- Regional anesthesia offers several advantages over general anesthesia, including reduced risk of complications such as postoperative nausea and vomiting, faster recovery times, and improved pain control postoperatively.
- By targeting specific nerves, regional anesthesia can provide effective pain relief while minimizing the dose of systemic medications, reducing the risk of side effects and complications.
5. Monitoring and Safety:
- Patients undergoing regional anesthesia are closely monitored throughout the procedure to ensure their safety and well-being.
- Monitoring typically includes assessment of vital signs, such as heart rate, blood pressure, and oxygen saturation, as well as continuous evaluation of the patient's level of consciousness and comfort.
6. Postoperative Care:
- After surgery, patients receiving regional anesthesia may experience numbness or weakness in the affected area as the effects of the local anesthetic wear off.
- Pain management strategies, including oral medications or additional nerve blocks, may be implemented to manage postoperative discomfort and promote recovery.
Regional anesthesia is a type of anesthesia that involves blocking nerve sensation in a specific region of the body to provide pain relief during surgical procedures. Unlike general anesthesia, which renders the patient unconscious, regional anesthesia allows the patient to remain awake or sedated while numbing the targeted area. Here's a detailed look at regional anesthesia:
1. Assessment and Diagnosis:
- Pain management begins with a comprehensive assessment of the patient's pain history, including the location, intensity, duration, and characteristics of pain.
- Healthcare providers use various tools, such as pain scales, questionnaires, and diagnostic tests (e.g., imaging studies, nerve conduction studies) to evaluate the underlying cause of pain and its impact on the patient's daily functioning.
2. Multidisciplinary Approach:
- Pain management services often involve a team of healthcare professionals with diverse expertise, including physicians (e.g., pain specialists, physiatrists, anesthesiologists), nurses, physical therapists, occupational therapists, psychologists, and social workers.
- This multidisciplinary approach allows for a holistic assessment of the patient's pain and the development of personalized treatment plans tailored to their specific needs.
3. Treatment Modalities:
- Pain management services utilize a variety of treatment modalities to address acute and chronic pain conditions. These may include:
- Medications: Analgesic medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, muscle relaxants, antidepressants, and anticonvulsants, may be prescribed to alleviate pain and improve function.
- Interventional Procedures: Minimally invasive procedures, such as nerve blocks, epidural injections, facet joint injections, radiofrequency ablation, and spinal cord stimulation, may be performed to target specific sources of pain and provide long-term relief.
- Physical Therapy: Exercises, manual therapy, modalities (e.g., heat, ice, ultrasound), and therapeutic techniques are employed to improve strength, flexibility, and mobility, and reduce pain-related disability.
- Psychological Therapy: Cognitive-behavioral therapy (CBT), relaxation techniques, mindfulness-based stress reduction (MBSR), biofeedback, and counseling are utilized to address the emotional and psychological aspects of pain, such as anxiety, depression, and coping strategies.
- Complementary and Alternative Therapies: Acupuncture, massage therapy, chiropractic care, yoga, tai chi, and herbal supplements may be recommended as adjunctive treatments to alleviate pain and enhance overall well-being.
4. Patient Education and Self-Management:
- Pain management services emphasize patient education and empowerment to facilitate self-management of pain and improve outcomes.
- Patients are educated about their pain condition, treatment options, potential risks and benefits, and strategies for pain relief and self-care.
- They are encouraged to actively participate in their treatment plan, set realistic goals, adopt healthy lifestyle behaviors (e.g., regular exercise, balanced diet, stress management), and engage in self-monitoring and self-regulation techniques.
5. Follow-Up and Long-Term Care:
- Pain management services provide ongoing follow-up and monitoring to assess treatment effectiveness, adjust interventions as needed, and address any complications or side effects.
- Long-term care focuses on maintaining functional improvement, optimizing pain control, preventing relapse, and enhancing overall quality of life.
Pain management services encompass a multidisciplinary approach to assess, diagnose, and treat acute and chronic pain conditions. These services are designed to improve patients' quality of life by addressing physical, emotional, and psychological aspects of pain. Here's a detailed look at pain management services:
Pediatric anaesthesiology focuses on providing safe and effective anesthesia for infants, children, and adolescents undergoing surgical procedures. Children have unique physiological and psychological needs that require specialized care and attention. The Pediatric Anaesthesiology team at Gleneagles HealthCity Chennai is trained to manage these challenges and create a child-friendly environment to alleviate anxiety and promote positive outcomes.
Obstetric anaesthesiology plays a crucial role in ensuring the safety and comfort of pregnant women during labor and delivery. This specialty involves administering anesthesia for pain relief during childbirth, as well as managing anesthesia-related complications in high-risk pregnancies. At Gleneagles HealthCity Chennai, obstetric anaesthesiologists work closely with obstetricians and midwives to provide comprehensive care for mothers and newborns.
Cardiac anaesthesiology specializes in providing anesthesia for patients undergoing heart surgery or interventional procedures. These may include coronary artery bypass grafting, valve replacement, or cardiac catheterization. Cardiac anaesthesiologists are trained to manage complex cardiovascular conditions and ensure hemodynamic stability during surgery.
Neuroanaesthesiology focuses on providing anesthesia for patients undergoing brain and spine surgeries or interventions. These procedures require precise management of intracranial pressure, cerebral blood flow, and neuro-monitoring to minimize the risk of neurological complications. Neuroanaesthesiologists at Gleneagles HealthCity Chennai are equipped with specialized knowledge and skills to navigate these complex procedures safely.
Organ transplantation is a complex surgical procedure that requires meticulous planning and coordination between multiple medical teams. Transplant anaesthesiologists play a critical role in optimizing the patient's condition before, during, and after transplantation. They are trained to manage the unique challenges associated with organ donation and transplantation, including immunosuppression and organ preservation techniques.
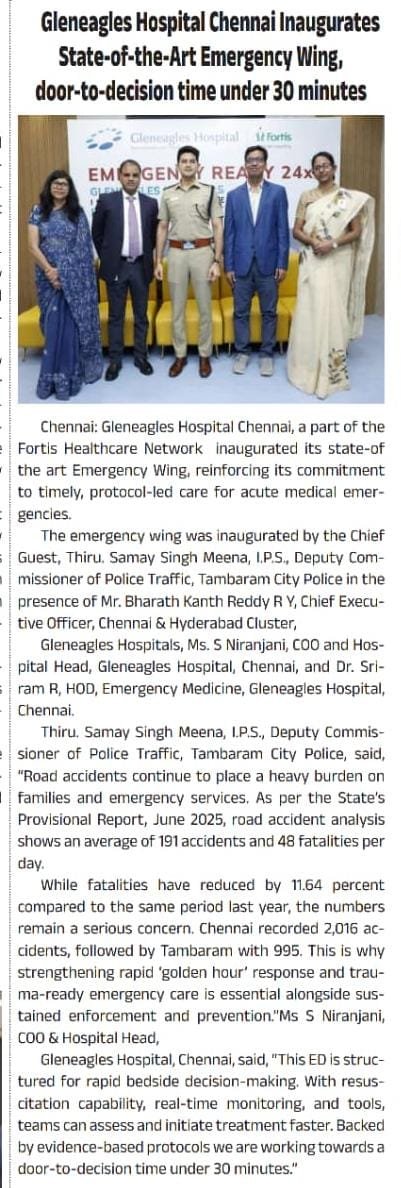
Emergency anaesthesiology involves providing rapid assessment and intervention for patients in life-threatening situations, such as trauma or cardiac arrest. The goal is to stabilize the patient's condition and ensure adequate oxygenation and circulation until further treatment can be initiated. Emergency anaesthesiologists at Gleneagles HealthCity Chennai are trained to respond swiftly and effectively to critical emergencies, both within the hospital and in the community.